
Finding a high-quality mental health IOP near me starts with understanding what an intensive outpatient program (IOP) actually provides and why it sits between weekly therapy and inpatient care. This guide explains how an IOP works, who benefits, and which conditions—like anxiety, depression, PTSD, and co-occurring disorders—are commonly treated in outpatient intensive programs. Readers will learn practical search tactics for local and virtual options, how to verify insurance coverage and costs, and how to compare IOPs with Partial Hospitalization Programs (PHP). The article maps evidence-based therapeutic modalities such as Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT), describes virtual IOP models and privacy safeguards, and offers checklists for evaluating local providers. By the end you will have a clear decision framework and concrete questions to ask prospective programs when searching for “mental health IOP near me,” ensuring informed choices that match clinical need and daily life constraints.
A mental health Intensive Outpatient Program (IOP) is a structured, non-residential level of care that delivers frequent therapy sessions and psychiatric support while allowing patients to live at home. IOPs increase treatment intensity through multiple weekly sessions—typically combining group therapy, individual therapy, and medication management—and they work by concentrating evidence-based interventions into a coordinated schedule. The primary benefit is intensive, multidisciplinary care without an overnight stay, which preserves community functioning and supports employment or schooling. This definition clarifies why a near-me search often prioritizes schedule flexibility and local coordination with outpatient providers. Understanding how IOP differs from other settings helps users choose an appropriate program level.
An IOP differs from traditional weekly outpatient therapy by offering several hours of treatment multiple days per week, whereas standard outpatient therapy generally consists of one session per week. IOPs provide higher treatment intensity and often include group skills training, psychiatry, and coordinated case management; this mechanism increases skill acquisition and symptom stabilization more rapidly than infrequent sessions. The specific benefit is faster functional improvement while avoiding inpatient admission. Comparing IOP with PHP and residential care clarifies who needs which level of support, and this comparison prepares readers to evaluate suitability and safety requirements.
Ideal IOP candidates include people experiencing moderate-to-severe symptoms that impair daily functioning yet do not require 24/7 medical supervision. Individuals with persistent depression, generalized anxiety, post-crisis step-down needs, or manageable co-occurring substance use often benefit because the program structure provides intensive therapy while preserving community supports. The mechanism of coordinated care—combining group skill-building with psychiatry—helps restore routines and supports work or school attendance. Recognizing these candidate profiles guides searchers when they look for “IOP for anxiety near me” or similar local services.
Typical IOPs run approximately 6–12 weeks with sessions held 3 days per week for 2–4 hours per day, though duration adapts to clinical progress and insurance parameters. This schedule concentrates evidence-based modules such as CBT and DBT skills, allowing measurable progress in coping skills and symptom reduction over weeks rather than months. The benefit is a predictable, intensive schedule that balances therapy intensity with real-life responsibilities. Knowing these ranges makes it easier to compare program expectations when investigating local options.

Mental health IOPs treat a broad set of diagnoses by delivering condition-tailored evidence-based therapies in group and individual formats. Programs commonly address mood disorders, anxiety disorders, trauma-related conditions, bipolar disorder, OCD, eating disorders, and co-occurring substance use, using targeted modules to address core symptoms and functional goals. The mechanism is modular treatment—skills groups plus individualized care—that yields symptom reduction and improved daily functioning. Understanding the condition coverage helps refine searches for “IOP for depression near me” or “IOP for PTSD near me” and informs questions to ask programs about their clinical expertise.
Mental health IOPs commonly treat the following conditions:
These condition categories guide the next step of exploring how IOPs apply specific therapies to each diagnosis and what outcomes to expect.
An IOP addresses anxiety by combining group CBT modules, exposure exercises, and skills training for panic, social anxiety, and generalized anxiety disorder. The mechanism uses repeated practice within groups to generalize coping strategies and reduce avoidance behavior through graded exposures. Benefits include measurable reductions in symptoms and improved daily functioning, often tracked with standardized anxiety scales. Understanding these components helps patients evaluate whether a local IOP offers the appropriate anxiety-focused curricula.
IOP treatments for depression commonly pair CBT and behavioral activation with psychiatric medication management when indicated, using structured modules to increase activity and address cognitive distortions. The mechanism of behavioral activation directly targets activity levels to reverse withdrawal and anhedonia, while CBT addresses dysfunctional thoughts that perpetuate depressive cycles. Expected benefits include improved mood, restored routines, and enhanced occupational or social functioning, which helps patients set realistic recovery goals when comparing local programs.
IOP can help with trauma and PTSD by first delivering stabilization and skills-based group work—often DBT-informed—before integrating trauma-focused individual therapies like cognitive processing or prolonged exposure when appropriate. The mechanism ensures safety by building emotion regulation and distress tolerance before trauma processing, reducing risk of destabilization. This layered approach benefits many trauma survivors while preserving access to community supports; assessing a program’s trauma-informed credentials is therefore essential when choosing nearby options.
Integrated IOP models treat co-occurring mental health and substance use disorders by coordinating addiction-focused interventions like relapse prevention with mental health therapies in the same program. The mechanism is joint treatment planning and multidisciplinary collaboration, which reduces fragmentation and improves adherence to both psychiatric and addiction interventions. Benefits include synchronized medication management, family therapy, and relapse-prevention skills that address dual-diagnosis complexity. Recognizing integrated approaches helps individuals seeking local programs that explicitly handle co-occurring conditions.
Mental health IOPs employ a combination of psychotherapy modalities, skills groups, and psychiatric services to address symptoms and functional goals. Common modalities include Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), group therapy, individual therapy, family therapy, and medication management, each contributing specific mechanisms that improve coping and reduce symptoms.
The primary benefit of this multimodal approach is comprehensive, coordinated care that addresses thought patterns, emotional regulation, interpersonal functioning, and biological contributors. Understanding modality roles makes it easier to compare program curricula when searching for “intensive outpatient program mental health” locally.
The following table summarizes major therapeutic modalities, how they are typically delivered in an IOP, and the expected benefits:
| Modality | Delivery | Expected Benefits |
|---|---|---|
| Cognitive Behavioral Therapy (CBT) | Group and individual sessions | Reduced maladaptive thinking, improved mood regulation, measurable symptom declines |
| Dialectical Behavior Therapy (DBT) | Group skills training, individual therapy | Enhanced emotion regulation, fewer crises, improved interpersonal functioning |
| Group Therapy | Peer interactions, skill rehearsal | Social support, shared experiences, enhanced coping strategies |
| Individual Therapy | Personalized treatment focus | Targeted interventions, deeper self-awareness, tailored coping skills |
| Family Therapy | Family involvement, systemic interventions | Improved family dynamics, support systems, relapse prevention |
| Medication Management | Psychiatric evaluation, medication coordination | Symptom stabilization, optimized pharmacotherapy, integrated care |
Programs use these modalities together to form a cohesive treatment plan that targets symptoms at multiple levels. The summary shows why looking for programs offering this mix is important when searching “mental health intensive outpatient program” near me.
CBT in IOP is delivered through structured group modules focused on cognitive restructuring, behavioral experiments, and homework assignments to change thought-behavior cycles. The mechanism relies on repeated in-session practice and between-session assignments to generalize skills to daily life. Benefits include reduced maladaptive thinking, improved mood regulation, and measurable symptom declines on standardized scales. Knowing CBT’s role assists in evaluating whether a program emphasizes evidence-based, measurable interventions.
DBT within IOP centers on skills training in mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness delivered mainly in group format with individual therapy for skill generalization. The mechanism helps individuals regulate intense emotions and reduce self-harm behaviors through concrete skills and coaching strategies. Benefits include stronger emotion regulation, fewer crises, and improved interpersonal functioning, making DBT-adapted IOPs especially suited for people with significant emotion dysregulation.
Group therapy provides peer feedback and repeated skills rehearsal, individual therapy personalizes treatment targets, and family therapy changes system-level dynamics that affect recovery. The mechanism combines social learning with individualized formulation and systemic adjustments, leading to more robust and durable change. Benefits include social support, targeted interventions for relationship issues, and alignment of family members in aftercare planning. These complementary formats enhance outcomes when programs integrate them coherently.
Medication management in IOPs typically involves psychiatric evaluation, medication initiation or adjustment, and coordination with therapists or external prescribers to align pharmacotherapy with psychotherapy. The mechanism is integrated care—psychiatrists or nurse practitioners work with therapists to ensure medications support therapeutic goals and functional recovery. Benefits include symptom stabilization that enables better participation in therapy and clearer measurement of combined treatment outcomes. Verifying on-site psychiatry or referral pathways is a key question when assessing local programs.
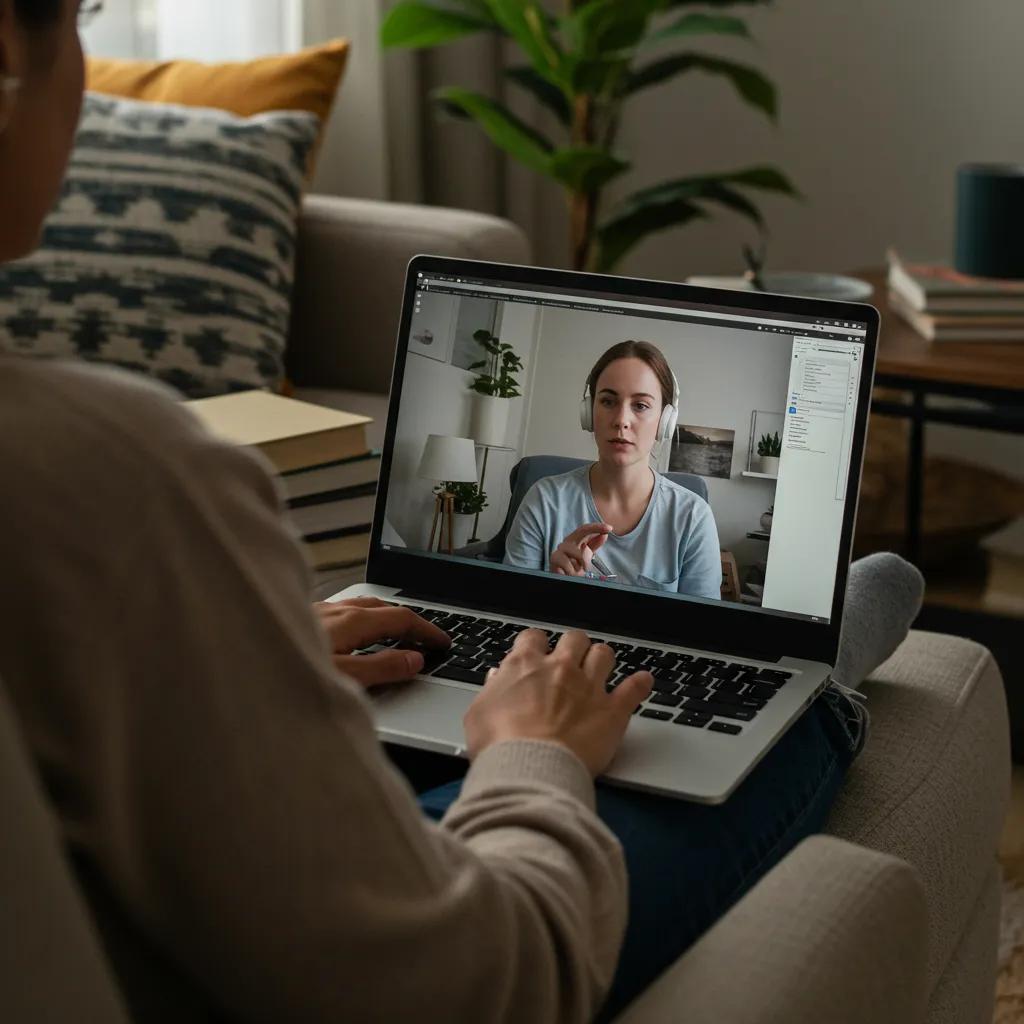
Virtual mental health IOP delivers the same core modalities—CBT, DBT, group skills, and psychiatry—through secure telehealth platforms, allowing participants to connect from home while maintaining intensive schedules. The mechanism mirrors in-person programs by preserving group interaction and clinician oversight, and recent studies through 2024–2025 indicate comparable effectiveness for many conditions when technology and engagement are adequate. The main benefit is increased access for people in underserved areas or with mobility or scheduling constraints, while maintaining structured treatment. Evaluating virtual program technology and privacy safeguards informs whether a near-me search should include remote options.
Virtual IOP increases access for rural or mobility-limited individuals and reduces commute time, enabling consistent attendance and integration with daily responsibilities. The mechanism improves retention by lowering logistical barriers and can expand access to specialized curricula that may not exist locally. Benefits include flexible scheduling and the ability to remain in one’s home environment while receiving intensive care. However, assessing technology requirements and engagement strategies is important before choosing virtual options.
Privacy and security in virtual IOP are ensured through HIPAA-compliant telehealth platforms, encrypted communications, informed consent processes, and secure documentation practices. The mechanism protects patient confidentiality via authentication controls and clinician training on virtual boundaries. Patients should ask providers about platform compliance, data storage policies, and emergency protocols to confirm safeguards. Understanding these safeguards helps users decide whether virtual delivery meets their confidentiality and safety needs.
Virtual IOP can treat many conditions such as anxiety, depression, and certain trauma-related disorders when acute safety needs are not present and local emergency supports can be coordinated. The mechanism relies on remote delivery of evidence-based therapies and local crisis planning to manage risk. Benefits include continuity of care and access to specialized providers for conditions that do not require in-person medical supervision. For high-risk situations like active suicidality, in-person or higher-acuity care may be necessary.
Selecting the right IOP involves targeted search strategies, verifying clinical credentials, assessing program structure, and confirming logistical fit with life demands. Start by searching directories and telehealth providers for “mental health IOP near me” and narrowing options by modalities offered, staff credentials, and insurance acceptance. The mechanism of a structured evaluation—asking standardized questions and reviewing outcome tracking—reduces selection error and increases the likelihood of a good match. Below is a concrete question list to use during intake calls and site visits.
These questions clarify clinical scope and logistical fit so you can compare programs systematically and move to cost verification.
Verifying coverage requires methodical steps: obtain service CPT/HCPCS codes or program descriptions, call the insurer with those codes, and confirm pre-authorization and out-of-pocket responsibilities. The mechanism of code-based verification ensures accurate benefit determinations and prevents surprise bills. Below is a checklist table to use when contacting insurers and providers.
| Insurance Type | What to Ask | Typical Coverage Details |
|---|---|---|
| Private employer plan | Ask for coverage of IOP services using CPT/HCPCS codes and pre-authorization requirements | May cover sessions with co-pay or coinsurance; prior authorization often required |
| Medicaid/CHIP | Ask whether the plan covers IOP and which providers are in-network | Coverage varies by state; many plans cover IOP with documentation of medical necessity |
| Medicare | Ask about outpatient mental health coverage and whether facility-based IOP is reimbursed | Medicare covers outpatient mental health; supplemental policies affect cost-sharing |
| Self-pay/Sliding scale | Ask about flat program fees, per-session billing, and financial assistance options | Some programs offer sliding scale or payment plans for uninsured patients |
After verifying codes and cost structures, ask the provider for a written estimate and explore payment plans or community mental health resources if needed. These steps minimize unexpected expenses and guide negotiation with insurers.
Quality indicators include licensed multidisciplinary staff, use of evidence-based therapies, routine outcome measurement, transparent admission criteria, and robust aftercare planning. The mechanism linking these indicators to better outcomes is coordinated professional care that monitors progress and adapts treatment. Benefits of choosing programs with these attributes include improved safety, clearer expectations, and stronger long-term gains. Verifying these signs during intake calls or site visits helps you differentiate high-quality local providers from lesser-equipped programs.
Effective aftercare planning connects IOP graduates with community therapists, peer support groups, vocational services, and crisis resources to maintain gains and prevent relapse. The mechanism involves discharge planning, referral coordination, and warm handoffs to outpatient providers to preserve continuity of care. Benefits include sustained recovery, reduced readmission rates, and strengthened social supports. Asking programs about their local resource networks clarifies how transitions will be managed when you search for nearby support options.
Mental health IOPs deliver measurable improvements in symptom severity, coping skills, and functional outcomes by concentrating evidence-based therapies into an intensive, coordinated plan. Recent research through 2024–2025 shows that structured IOPs, including telehealth variants, achieve symptom reduction and functional gains comparable to higher levels of care for appropriately selected patients. The mechanism is multimodal intervention—therapy, skills training, and medication coordination—which produces durable behavior change. Understanding typical benefits and success metrics helps set expectations when comparing programs locally.
Common benefits observed in IOP outcomes include:
These outcome domains indicate why many patients prefer IOP when inpatient care is unnecessary.
IOP improves coping skills by providing repeated practice of evidence-based techniques—such as DBT emotion regulation and CBT cognitive restructuring—within groups and individual sessions that scaffold skill acquisition. The mechanism of guided practice plus homework leads to generalization into everyday situations, producing measurable changes in behavior and emotion management. Benefits include fewer crises, better stress response, and greater self-efficacy. Recognizing these mechanisms clarifies why skills-based modules are central to most IOP curricula.
Evidence supporting IOP effectiveness includes randomized and observational studies demonstrating that structured outpatient intensives reduce symptoms and improve functioning for depression, anxiety, and certain trauma-related conditions; telehealth outcome studies from 2020–2025 show comparable results when programs maintain engagement and platform security. The mechanism is consistent application of evidence-based therapies in a sufficiently intensive dose to produce clinical change. These research findings provide a reasonable expectation of benefit for qualified candidates and support the inclusion of virtual options in a near-me search.
Ethical presentation of success stories uses anonymized vignettes—challenge, treatment, outcome—supported by outcome measures rather than sensational claims, illustrating typical recovery trajectories like reduced depressive symptoms and return to work. The mechanism of anonymized composites protects privacy while conveying realistic expectations for improvement. Benefits of these stories include helping prospective patients envision recovery steps and commitment required. When providers offer such vignettes, verify they follow ethical standards and measure outcomes objectively.
An IOP differs from a Partial Hospitalization Program (PHP) primarily in intensity, daily hours, and medical supervision levels; PHP commonly offers full-day treatment with greater clinical monitoring and access to medical staff. The mechanism distinguishing them is the degree of supervision and frequency of therapeutic contact, which dictates suitability for higher-acuity needs. The benefit of comparing IOP and PHP is choosing the correct level of care to match safety and clinical requirements. A concise comparison helps users quickly determine which program aligns with current needs.
The following table provides a side-by-side comparison to guide decisions:
| Program | Intensity (hours/week) | Typical Duration | Best Suited For |
|---|---|---|---|
| Intensive Outpatient Program (IOP) | ~6–12 hours/week | 6–12 weeks | Patients needing intensive therapy but safe at home |
| Partial Hospitalization Program (PHP) | ~20+ hours/week | Several weeks to months | Patients requiring closer monitoring without inpatient admission |
| Inpatient/Residential | 24/7 care | Variable | High acuity, safety needs, or medical stabilization |
This comparison clarifies when to seek PHP over IOP based on safety and support requirements.
IOP typically provides several weekly sessions totaling a few hours per day, while PHP offers half- to full-day treatment with greater access to nursing and medical staff; this structural difference reflects differing levels of supervision and intervention. The mechanism is intensity-driven: higher hours and medical resources in PHP address greater acuity and medical needs. Benefits of this clarity include appropriate triage to the level of care that ensures safety and maximizes therapeutic benefit. Understanding these differences informs whether local search results for “mental health day treatment near me” should prioritize PHP listings.
Choosing between IOP and PHP depends on safety, level of daily functioning, need for medical supervision, and support at home; red flags for PHP include active suicidality, severe medical comorbidity, or inability to meet daily needs. The mechanism for making this decision is clinical assessment—preferably by a licensed clinician—using symptom severity, risk factors, and support availability. Benefits of a proper match include faster stabilization and reduced risk of relapse. If uncertain, arrange an assessment with a local provider or telehealth clinician to determine the appropriate level of care.
We are 100% in Network Provider. Most of our clients pay $0 out of pocket.



